What are adrenal or suprarenal tumors?
The adrenal glands, also known as suprarenal glands, are located near the spine and large blood vessels, close to the top of the kidneys, and are part of the endocrine system. Divided into medulla and cortex, they are responsible for producing substances that control the circulatory system (catecholamines) and hormones that act on both metabolism processes (such as cortisol) and sexual function (androgens).
When the cells of the medulla or cortex proliferate uncontrollably, adrenal tumors occur. This growth is due to genetic mutations that are not corrected by the body.
Because they are very rare, it has not yet been defined what the risk factors for adrenal tumors may be. The presence of some genetic syndromes seems to predispose the development of both malignant and benign tumors:
- Multiple endocrine neoplasia type 2 (MEN2);
- Neurofibromatosis type 1 (Von Recklinghausen disease);
- Beckwith-Wiedemann syndrome;
- Li-Fraumeni syndrome;
- Paraganglioma syndrome (extra-adrenal pheochromocytoma); and
- Von Hippel-Lindau syndrome.
Adrenal tumors are not always malignant: the occurrence of benign tumors is more frequent in these cases. Next, we will address the two types of malignant adrenal tumors.
Subtypes of adrenal tumors
When malignant, the adrenal tumor can be of two types: adrenal carcinoma (or adrenocortical carcinoma) and pheochromocytoma.
Adrenal carcinoma or adrenocortical carcinoma is a tumor that originates in the cortex of the adrenal gland itself. In most cases, it is non-functioning, but it can present hyperfunctioning in a small portion of occurrences.
It is a rare tumor, with an annual incidence of 1 to 2 cases per 1 million people. It affects men and women equally and has three peaks of occurrence:
- Children aged 1 and 2 years;
- Children between 7 and 16 years;
- Adults aged 50 years and older (more common).
In most cases (50% to 70%), the disease affects the left adrenal gland, and in 5% to 7% of occurrences, it is bilateral.
Pheochromocytoma is a tumor that originates in the medulla of the adrenal gland and is extremely rare. Its most frequent sites of dissemination are lymph nodes, lungs, liver, and bones.
There is a subtype of pheochromocytoma, called paraganglioma, which is ectopic or extra-adrenal, arising from para-aortic sympathetic ganglia.
Even rarer than adrenal carcinoma, pheochromocytoma has a very low incidence, occurring in 0.05% to 0.1% of hypertensive patients. Its peak incidence is from 30 to 40 years of age, but it can occur in younger people when associated with hereditary syndromes – in these cases, it tends to be more aggressive and have a higher probability of metastasis. It is usually bilateral.
Symptoms and signs of adrenal tumors
Benign adrenal tumors are generally asymptomatic, as are malignant tumors in early stages. However, malignant tumors in more advanced stages often have symptoms similar to other types of cancer, such as:
- Fatigue;
- Unexplained weight loss;
- Abdominal mass;
- Blood in the urine;
- Fever;
- Anemia;
- Abdominal pain.
Symptoms directly related to adrenal carcinoma include menstrual cycle changes, acne development, and skin fragility, while typical signs of pheochromocytoma are those related to the release of catecholamines and metabolites of adrenaline and noradrenaline: hypertension, arrhythmia, and/or hyperglycemia.
In children, the most common symptoms are caused by male hormones that the tumor can produce: excessive growth of facial and body hair, enlargement of the penis and breasts in boys, and enlargement of the clitoris in girls.
Diagnosis of adrenal tumors
When noticing symptoms and seeking a doctor’s help, the patient will need to undergo several tests to confirm adrenal tumors.
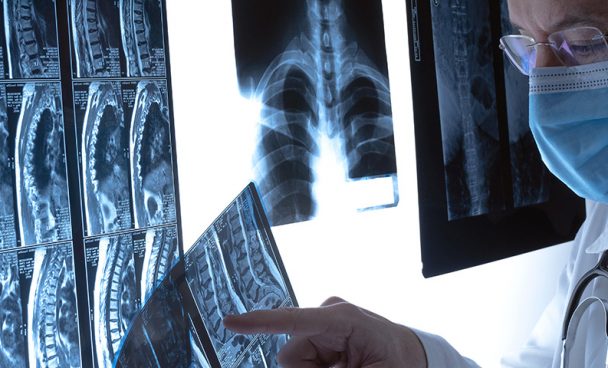
Usually, blood and urine tests are requested to analyze hormone levels, along with abdominal imaging tests. Ultrasound can identify changes in adrenal size, and more specific tests, such as computed tomography (CT), magnetic resonance imaging (MRI), and PET scans, can complement the study of the lesions.
Adrenal carcinoma is often diagnosed when the disease reaches a volume larger than 6 cm. MRI is the most accurate method to evaluate it.
For pheochromocytoma, the evaluation tends to be through laboratory measurements (blood and urine) of possible adrenaline, noradrenaline, and catecholamine metabolites (although about 15% to 20% of patients have normal catecholamine levels). Elevated levels are generally diagnostic of the disease.
Adrenal tumors are usually diagnosed early when a CT scan is performed for another health issue – in other words, detection is accidental. The specific diagnosis is usually at a more advanced stage, with the onset of symptoms, when tumors begin to press on other organs.
Treatment for adrenal tumors
The treatment for adrenal tumors depends on their location, size, and the patient’s clinical condition. Initially, it is common to perform surgery to remove one or both adrenal glands – the procedure is called adrenalectomy. It can be minimally invasive, using robotic surgery and laparoscopy, or open surgery.
Radiation therapy, chemotherapy, and the use of other medications may complement the treatment of adrenal tumors after surgery. When surgery is not possible, systemic chemotherapy can be used.
Prevention of adrenal tumors
While there is a wide range of tests available for diagnosis, there is no routine screening for adrenal tumors. If you experience symptoms, you should consult with a urologist or oncologist for further evaluation.